https://docs.google.com/etc
Abscesses:
- result from wounds sustained at least 3 days ago
- Step 1: surgical debridement
- don gloves and face mask
- surgically prep the puncture site
- use scalpel blade or hypodermic needle to lance abscess usually where original puncture was
- empty the abscess
- lavage with 1:40 dilution of Chlorhexidine
- remove necrotic tissues
- suture edges of wound if it's large
- create 2 new holes for Penrose drain to enter and exit, keep gravity in mind when choosing the location
- insert drain and suture on both ends
- clean drain site daily
- remove drain within 3 days
- remove drain as you would sutures so that nothing that's been outside the wound gets drug back through the wound upon removal
- Step 2: medical treatment
- antibiotics
- HR: below 80Bpm
- RR: below 12 bpm
- CRT: under 1sec or over 2sec
- T: under 99F or more than a 2 degree drop
- Doppler, Systolic: below 100mmHg
- Doppler, Oscillometric: below 80mmHg
- CVP: 8cmH2O
- ET CO2: less than 25mmHg or over 45mmHg
- SpO2: 90%
- Autoclave 121C/250F 15 PSI 15min
- Flash Autoclave 133C/272F 35PSI 1min
- Detergents:
- Ethylene Oxide 1-18hrs + 24-48hrs to vent
- NOT inactivated by organic materials: Phenols (Pine-Sol), Biguanides (Chlor-Hex)
- Sporicidal: Chlorine (Bleach), Aldehydes (Cidex)
- Scrubbing:
- fingernails
- wash w/ soap
- scrub fingertips, fingers, then hand on hand #1 (20 strokes on each surface)
- scrub fingertips, fingers, then hand on hand and wrist area of hand #2
- scrub wrist area of arms, then elbow area of arm #1
- scrub elbow area of arm #2
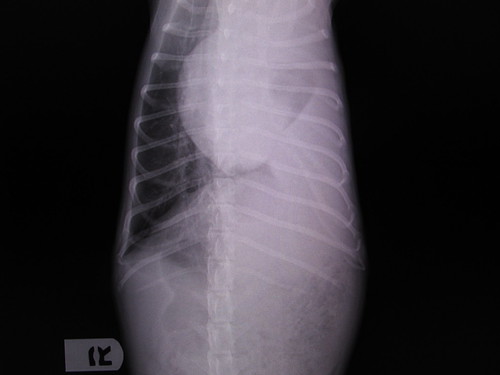
- start in right lateral recumbency
- do compressions about where the elbow rests
- at costochondral junction
- compress no more than 30% to avoid cracking ribs
- thoracic pump: do compressions in time with breaths
- in dorsal recumbency, compressions are done on caudal end of sternum and at an angle down and cranial
- never stop for more than 10sec for any reason
- compressions contraindicated with:
- rib fracture
- pleural effusion
- pneumothorax
- cardiac tamponade
- Analgesics:
- Ketamine/Telazol
- A2A's
- Butorphanol
- Controlled:
- Diazepam
- Torbutrol
- Butorphanol
- Morphine and derivatives
- Fentanyl
- Ketamine
- Manometer max for giving breath: 20cmH20/14mmHg
- Manometer max for regular use: 4cmH20/2-3mmHg
- F-tubes: blue inner tube = inspiration, clear outside = exhalation
- Staining:
- Black/White spots = minerals in water
- Corrosion = wet, dry time cut short?
- Rust deposits = hard water, corrosion
- Blue/Grey = reverse metal plating, in cold sterile too long, chlorhex residue, exposure to saline?
- Brown/Orange w/o pitting = iron in water, high pH detergent
- Dark Brown = dried blood
- Multi-color = excessive heat exposure
- Read flow meter at center of ball, or at top of bobbin. If there are 2 balls, there should be 2 scales, the top ball will read on the smaller scale, the bottom on the larger scale.
- APM, Audio Patient Monitor: esophageal stethoscope w/ speaker to amplify the sound.
- Direct BP monitor(MAP, Mean Arterial Pressure -most accurate) inside body (uncommon),atrial or CVP which must be measured on expiration.
- Indirect BP monitor = Doppler or Sphagnometer: hold the part with the reading at the animal's heart level; the 1st sound is systolic, 2nd is diastolic; not accurate, so take 5 readings, eliminate the highest and lowest, then average the other 3.
- Ocillometer -gives digital readout, measures size change. Cuff size: width more important than circumference, width should be 40% of the circumference of the limb it will be used on.
- Laser: Think of the laser workpiece as looking like a mechanical pencil. If you take the lead out, the "lead" is the tip and the empty pencil is the laser handpiece.
- # of L of O2 left in an H tank: psi x 3.3
- # of L of O2 left in an E tank: psi x 0.3
- Reservoir bag: 5-6 x tidal volume, always round up
- Tidal volume: 10ml/kg minimum
- 2.5% = 25mg/mL
- 1:1000 = 1g/L? = 1mg/mL?
- max lidocaine for cats= 4mg/kg (3 spots per paw)
- fluid deficits = % lost x kg (10% of 20kg = 2kg = 2L lost)
- Fluid rates
- shock in dogs = 60-90ml/kg/hr
- shock in cats = up to 60ml/kg/hr
- maintenance = 40-60ml/kg/day
- surgery = 10ml/kg/hr
- drip rate: (calibration x volume)/time
- max potassium rate =0.5meq/kg/hr
Oxygen supplementation:
- flow-by
- face mask
- nasal prongs
- tube pointed at nose/mouth
- oxygen tent
- zip-lock bag
- e-collar
- oxygen cage
- nasal catheter -for longer term administration
- numb nostril
- measure tube from nose to medial canthus
- mark tube w/ tape
- lube tube
- insert tube when at leats 4min have passed since numbing
- suture a loop next to the nose
- suture tape on tube to suture loop through skin
- secure tube above forehead with tape?, glue? or more suture
- simple interrupted -J-J-J-
- uninterrupted/continuous -/-/-/-
- horizontal mattress = = =
- vertical mattress -| -| -|-
- cruciate/cross mattress -X-X-X-
- Airway
- make sure patent
- clear obstructions
- place ET tube
- Heimlich?
- tracheostomy?
- Breathing
- O2 supplementation
- manual ventillation?
- mouth to snout?
- Circulation
- IV catheter, fluids
- hemorrhage control
- CPR
- Drugs
- bolus IV drugs with 10-20cc saline
- dilute intratracheal drugs with 5-10cc sterile water
- Exam/Electrical Defibrillation
- defibrillation is only for v-fib or v-tach
- Follow-up
- Immediate:
- airway obstruction
- cardiac or respiratory arrest
- DOA
- Critical:
- respiratory or cardiac distress (pulmonary edema, arrhythmias)
- shock
- active bleeding (arterial or venous)
- active seizuring
- Serious:
- large wounds, compound fractures, traumatic injury
- bloat (GDV)
- toxin ingestion
- blocked male cats
- puppy and kitten sickness/weakness
- Less Serious:
- fractured tooth, toenail injury, URI, etc
- MAC: high MAC = high safety = less potent = more required to maintain anesthesia
- Methoxyflurane is nephrotoxic
- Halothane is hepatotoxic
- Intubation:
- size according to width of space between nares
- ready one size smaller as well just in case
- check for leaks
- measure to thoracic inlet on the animal
- lube
- push epiglottis down with ET tube
- push down while inserting tube between arytenoid cartilage/vocal folds and into trachea
- tie in
- verify it's in place:
- watch for fogging INSIDE the tube
- palpate neck, if you feel 2 tubes, it's in the esophagus
- watch for bag movement during breathing
- listen to lung sounds on both sides
- Prep:
- cat spay: midway between umbilicus and pubis bone
- dog spay: 1/4 to 1/3 down from umbilicus
- Review nerve block sites
- Monofilament:
- less traumatic to tissues
- does not wick
- Multifilament:
- greater strength
- holds knots better
- less memory (easier to work with)
- Storage times for packs: 4w muslin, 6m paper, double if double-wrapped
- Black handled instruments are "extra sharp", but dull more quickly.
- Gold handled instruments hold their edge longer and have stronger gripping surfaces
- Osteotome has a point at it's center, slices bone.
- Bone chisel has it's point off-center and is used to chip away bone.
- O2 flow by: connect O2 to flow meter to outlet to patient (ET tube, mask, etc)
- ECG:
- measuring mv: 10cm = 1mv (at standard calibration)
- if not standard, squared off wave = 1mv
- complexes are measured in height (mv) and width (sec)?
- intervals are measured in width (sec) only ?
- lead placement
- front: just proximal to elbow (on the caudal aspect)
- rear: just proximal to stifle (on cranial aspect)
- precordial clip goes on end of sternum
- Tourniquet placement:
- front: proximal to elbow, metal clasp over tricep (caudal aspect, not medial or lateral)
- rear: proximal to knee, metal clasp lateral or medial (check)
- Landmarks for Ortolani's sign: ischium and greater trocanter